from NYT > Health https://ift.tt/mCJkV3B
 December 31, 2022
December 31, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/mCJkV3B
 December 31, 2022
December 31, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/GdqHNQO
 December 30, 2022
December 30, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

Here are some suggestions from the American Medical Association (AMA) that pack the most punch.
from WebMD Health https://ift.tt/gtASLFR
 December 30, 2022
December 30, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

Relapsing-remitting multiple sclerosis can happen to anyone. But there are disparities when it comes to certain racial and ethnic groups.
from WebMD Health https://ift.tt/YSgprjC
 December 30, 2022
December 30, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

In November, actor Chris Hemsworth announced that he would be taking a leave from acting to focus on other things after discovering he has a genetic vulnerability to Alzheimer’s disease. Here's what to know.
from WebMD Health https://ift.tt/P2QuloI
 December 30, 2022
December 30, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

While 8 of 10 mothers breastfeed their newborns for a short time, the number plummets despite recommendations from experts, in part because milk production falls off.
from WebMD Health https://ift.tt/pra6M8v
 December 30, 2022
December 30, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments
New research suggests that adding climate-impact labeling to fast-food menus can have a big effect on whether or not consumers go “green" when eating out.
from WebMD Health https://ift.tt/YOq3onj
 December 29, 2022
December 29, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/65fbAjp
 December 29, 2022
December 29, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

In a small study, a simulated driving program helped to reduce the crash risk for teens with ADHD.
from WebMD Health https://ift.tt/lvWJ2Cp
 December 29, 2022
December 29, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments
As holiday celebrations wind down in the U.S., COVID is on the rise, even as people head out to ring in what they hope will be a healthier new year. While many would like to take a vacation from even thinking about COVID, the question of what's next with COVID is always looming. Here's what to know.
from WebMD Health https://ift.tt/DSVW4dZ
 December 29, 2022
December 29, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/rXYivJH
 December 28, 2022
December 28, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/JSYiosk
 December 28, 2022
December 28, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

Here’s what to know about the services and accommodations offered by school districts to children with SMA Type 3 and how to best advocate for your child.
from WebMD Health https://ift.tt/0kGyq3R
 December 28, 2022
December 28, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

A new study raises concerns over pediatric poisonings from a particularly lethal combo — a potent synthetic opioid known as fentanyl and a powerful veterinary sedative called xylazine.
from WebMD Health https://ift.tt/IvmNskh
 December 28, 2022
December 28, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

While it’s often the case that great business ideas emerge from personal experiences, when a health issue prompts the development of a company, the results can be incredible for both the founder and customers, too. Such was the case for these four CEOs who transformed their own personal health journeys into businesses that have helped so many women along the way. Here are their stories.
from WebMD Health https://ift.tt/9hQ6oXU
 December 28, 2022
December 28, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

New research finds many Asian American and Native Hawaiian/Pacific Islander adults may have trouble accessing health care and insurance because of language barriers.
from WebMD Health https://ift.tt/NFJt0PA
 December 27, 2022
December 27, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

Find out what’s best to wear to prevent and manage chronic spontaneous urticaria (CSU), also called chronic hives.
from WebMD Health https://ift.tt/4HJqAmK
 December 27, 2022
December 27, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

Georgia Tech engineers have developed AI that can identify diarrhea with up to 98% accuracy and could help us catch disease outbreaks early.
from WebMD Health https://ift.tt/gW0IQZp
 December 27, 2022
December 27, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

Find out what’s best to wear to prevent and manage chronic spontaneous urticaria (CSU), also called chronic hives.
from WebMD Health https://ift.tt/LhvONyX
 December 27, 2022
December 27, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/gVSLxld
 December 27, 2022
December 27, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

When you have pulmonary arterial hypertension, it’s important to see your doctor regularly to make sure everything is OK. Here’s what to expect.
from WebMD Health https://ift.tt/uOmX3l5
 December 27, 2022
December 27, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/eWY1RIi
 December 26, 2022
December 26, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/VDzqWiG
 December 26, 2022
December 26, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/SqL0lIZ
 December 26, 2022
December 26, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

What’s it like living with psoriatic arthritis for a Black woman. Find out one woman’s diagnosis journey.
from WebMD Health https://ift.tt/KPbW3fy
 December 26, 2022
December 26, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

Psoriatic arthritis hitting the wall, moving forward with psoriatic arthritis, tips for living with psoriatic arthritis
from WebMD Health https://ift.tt/MFzZQYg
 December 26, 2022
December 26, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/blnCy5N
 December 24, 2022
December 24, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/tzKHde3
 December 23, 2022
December 23, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

The CDC reports in 2019 the average American could have expected to live an average of 78.8 years, life expectancy declined to 77 years in 2020, and then to 76.4 years in 2021.
from WebMD Health https://ift.tt/uLR6jcU
 December 23, 2022
December 23, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
Oldways Ambassadors Brenda Atchison and Glorya Fernandez walked a KHN reporter through two cooking demonstrations to showcase modern takes on cultural classics — like a cold black-eyed pea salad just in time for the new year, and a garlicky dill mojo sauce served over spinach salad.
Last year, Kelly LeBlanc, director of nutrition at Oldways, shared the organization’s heritage-based food guide pyramids with KHN for a report on USDA food guidelines. It’s the 10-year anniversary of Oldways’ A Taste of African Heritage nutrition curriculum, and this year, the curriculum became part of the Department of Agriculture’s SNAP-Ed Toolkit, a collection of interventions from the Supplemental Nutrition Assistance Program educational effort focused on helping low-income households make healthier food choices and reinforce healthy eating habits.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/XAnUyWd
 December 23, 2022
December 23, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/KW1IQmZ
 December 22, 2022
December 22, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
LUMPKIN, Ga. — En octubre, Yibran Ramirez-Cecena no le dijo al personal del Centro de Detención de Stewart que tenía tos y secreción nasal. Está detenido en la instalación del suroeste de Georgia desde mayo, y ocultó sus síntomas por temor a que lo pusieran en confinamiento solitario si daba positivo para covid-19.
“Honestamente, no quería pasar 10 días solo en una habitación, lo llaman el agujero”, dijo Ramírez-Cecena, quien espera que decidan si es deportado a México o puede permanecer en los Estados Unidos, en donde ha vivido por más de dos décadas.
Poco antes de que Ramírez-Cecena se enfermara, los funcionarios del Servicio de Inmigración y Control de Aduanas (ICE) de la instalación le negaron su solicitud de alta médica. Es VIH positivo, que según la lista de los Centros para el Control y la Prevención de Enfermedades es una afección que puede aumentar el riesgo de enfermar gravemente por covid.
Ahora, frente al tercer invierno pandémico, reza para no contraer covid mientras está detenido. “Todavía da miedo”, dijo.
En todo el país, la posibilidad de desarrollar una enfermedad grave o morir por covid ha bajado, por las vacunas de refuerzo actualizadas, las pruebas en el hogar y las terapias. La mayoría de las personas pueden sopesar los riesgos de asistir a reuniones o viajar.
Pero para las aproximadamente 30,000 personas que viven en espacios cerrados en la red de instalaciones de inmigración del país, covid sigue siendo una amenaza constante.
El ICE actualizó su guía de pandemia en noviembre. Pero las instalaciones han ignorado las recomendaciones anteriores de usar máscaras y equipo de protección, tener pruebas y vacunas disponibles, y evitar el uso del confinamiento solitario como cuarentena, según detenidos, grupos de defensa e informes internos del gobierno federal.
Según los protocolos de ICE, el aislamiento por covid, utilizado para evitar que otros detenidos se enfermen, debe estar separado de la segregación disciplinaria.
La agencia no abordó este punto, pero dijo en un comunicado a KHN que a los detenidos se los coloca en una “sala de alojamiento médico individual” o en un “una habitación de aislamiento médico de infecciones transmitidas por el aire”, cuando esté disponible.
La atención médica en los centros de detención de inmigrantes ya era deficiente antes de la pandemia. Y en septiembre, las personas médicamente vulnerables en los centros de detención de ICE perdieron una protección, con la expiración de una orden judicial que requería que los funcionarios federales de inmigración consideraran la liberación de los detenidos con riesgo de covid.
La agencia “ha renunciado por completo a proteger a las personas detenidas de covid”, dijo Zoe Bowman, abogada supervisora de Las Américas Immigrant Advocacy Center en El Paso, Texas.
El uso de la detención de inmigrantes en el país se disparó a fines de la década de 1990 y creció después de la creación de ICE en 2003. Los centros de detención —unos 200 complejos privados, instalaciones administradas por ICE, cárceles locales y prisiones repartidas por todo el país— retienen a adultos que no son ciudadanos estadounidenses mientras disputan o esperan la deportación.
La duración promedio de la estadía en el año fiscal federal 2022 fue de aproximadamente 22 días, según la agencia. Los defensores de los inmigrantes han argumentado durante mucho tiempo que las personas no deberían ser detenidas y, en cambio, se les debería permitir vivir en comunidades.
El Centro de Detención de Stewart, un vasto complejo rodeado de cercas con alambre de púas en los bosques de Lumpkin, tiene una de las poblaciones de detenidos más grande del país. Cuatro personas bajo la custodia del centro han muerto por covid desde el comienzo de la pandemia, el mayor número de muertes por covid registradas en estos centros.
Cuando funcionarios de inmigración transfirieron a Cipriano Álvarez-Chávez al centro de Stewart en agosto de 2020, todavía confiaba en la máscara que tenía después de ser liberado de la prisión federal en julio, según su hija, Martha Chavez.
Diez días después, el sobreviviente de linfoma de 63 años fue llevado a un hospital en Columbus, a 40 millas de distancia donde dio positivo para covid, según su informe de defunción. Murió después de pasar más de un mes conectado a un ventilador.
“Fue pura negligencia”, dijo su hija.
Dos años después de la muerte de Álvarez-Chávez, grupos de defensa y detenidos dijeron que el ICE no ha hecho lo suficiente para proteger de covid a los detenidos, una situación consistente con el historial de atención médica deficiente y falta de higiene de las instalaciones.
“Es desalentador ver que no importa cuánto empeoran las cosas, nada cambia”, dijo la doctora Amy Zeidan, profesora asistente en la Facultad de Medicina de la Universidad de Emory, quien revisa los registros de salud de los detenidos y realiza evaluaciones médicas para las personas que buscan asilo.
Una investigación bipartidista del Senado reveló en noviembre que las mujeres en el Centro de Detención del Condado de Irwin en Georgia “parecen haber sido sometidas a procedimientos ginecológicos excesivos, invasivos y, a menudo, innecesarios”.
En el Centro de Procesamiento de Folkston, también en Georgia, el ICE no respondió a las solicitudes médicas de manera oportuna, tuvo una atención de salud mental inadecuada y no cumplió con los estándares básicos de higiene, incluidos baños funcionales, según un informe de junio de la Oficina del Inspector General de Seguridad del Departamento de Asuntos Internos. Y una denuncia presentada en julio por un grupo de organizaciones de defensa alegó que una enfermera del centro Stewart agredió sexualmente a cuatro mujeres.
El ICE defendió su atención médica en un comunicado enviado por correo electrónico, diciendo que gasta más de $315 millones anualmente en atención médica, y que garantiza la prestación de los servicios médicos necesarios e integrales.
Aún así, muchas instalaciones carecen de personal y están mal equipadas para manejar las necesidades médicas a largo plazo de la gran población de detenidos, dijo Zeidan. La atención tardía es común, la atención especializada es casi inexistente y el acceso a la terapia es limitado, dijo. El cuidado de covid no es diferente.

En sus protocolos para covid, el ICE recomienda el uso de anticuerpos monoclonales, que ayudan al sistema inmunológico a responder de manera más efectiva a covid, para el tratamiento. Pero no reconoce ninguno de los otros tratamientos recomendados por los CDC, incluidos los antivirales como Paxlovid, que pueden reducir las hospitalizaciones y las muertes entre los pacientes con covid.
“Durante décadas, el ICE ha demostrado ser incapaz y no estar dispuesto a garantizar la salud y la seguridad de las personas bajo su custodia”, dijo Sofia Casini, directora de monitoreo y defensa comunitaria de Freedom for Immigrants, un grupo de defensa. “Covid-19 solo ha empeorado esta horrible realidad”.
Once personas han muerto por covid bajo custodia de ICE. Pero ese número puede ser una subestimación; defensores de los detenidos han acusado a la agencia de liberar a las personas o deportarlas cuando están gravemente enfermas como una forma de evadir las estadísticas de muertes.
Antes de la pandemia, Johana Medina León fue liberada de la custodia de ICE cuatro días antes de su muerte, según un artículo de mayo en Los Angeles Times. Vio a un médico unas seis semanas después de su primera solicitud, decía el artículo, pero ICE aceleró su liberación solo unas horas después de que su condición empeorara.
Este otoño, los detenidos recluidos en instalaciones de todo el país llamaron a la línea directa de detención de Freedom for Immigrants para quejarse de las condiciones de covid, que varían de una instalación a otra, dijo Casini. “Incluso en la misma instalación, puede cambiar de semana a semana”, dijo.
Según Casini, muchas personas que habían dado positivo para covid estaban recluidas en las mismas celdas que las personas que habían dado negativo, incluidas las personas médicamente vulnerables. Este verano, el grupo encuestó a 89 personas a través de su línea directa y descubrió que alrededor del 30% de los encuestados tuvieron problemas para acceder a las vacunas mientras estuvieron detenidos.
Ramírez-Cecena dijo que le dijeron que es elegible para una segunda vacuna de refuerzo de covid, pero que, a diciembre, aún no la había recibido. Un detenido en el Centro de Procesamiento de Moshannon Valley en Pennsylvania dijo que a un guardia se le permitió interactuar con los detenidos mientras estaba visiblemente enfermo, dijo Brittney Bringuez, coordinadora del programa de asilo de Physicians for Human Rights, quien visitó las instalaciones este otoño.
La orden judicial que requería que ICE considerara la liberación de personas con alto riesgo de covid ha ayudado a los detenidos con afecciones médicas graves, dijeron los defensores. Según la orden, ICE liberó a unos 60,000 detenidos médicamente vulnerables en dos años, dijo Susan Meyers, abogada sénior del Southern Poverty Law Center, uno de los grupos de defensa que ayudó a presentar la demanda que resultó en la orden judicial.
El ICE dijo en un comunicado que aún considerará los factores de riesgo de covid como una razón para la liberación. Pero los abogados dijeron que las instalaciones de ICE a menudo no cumplían con la orden judicial cuando estaba vigente.
El año pasado, el ICE negó la solicitud de liberación de Ricardo Chambers del Centro de Detención de Stewart. Chambers, de 40 años, tiene enfermedades psiquiátricas graves, consideradas un factor de riesgo según la orden judicial. También tiene problemas para respirar y se ahoga mientras duerme, como resultado de una lesión nasal que sufrió en un ataque antes de ser detenido. A dos años de estar detenido, todavía no recibió atención para esa lesión.
Ha presentado quejas sobre los protocolos para covid de Stewart, incluidas las condiciones de hacinamiento y la falta de uso de máscaras u otro equipo de protección por parte del personal.
Al negar su liberación, el ICE dijo que Chambers era una amenaza para la seguridad pública debido a sus antecedentes penales, según su abogada Erin Argueta, abogada principal de la oficina de la Iniciativa de Libertad de Inmigrantes del Sureste del Southern Poverty Law Center en Lumpkin. Chambers ya cumplió sus condenas, dijo, y hay una familia en Nueva York que lo acogería.
A principios de este año, fue enviado a confinamiento solitario durante unos 10 días después de dar positivo para covid, dijo. Pero Chambers, quien está luchando contra una orden de deportación a Jamaica, dijo que su experiencia con covid no fue diferente de las otras veces que estuvo en aislamiento.
“Serás tratado como un animal, enjaulado y sin tener culpa de nada”, dijo Chambers.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/BoCYPu1
 December 22, 2022
December 22, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/vfOqcoQ
 December 22, 2022
December 22, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
A group of emergency physicians and consumer advocates in multiple states are pushing for stiffer enforcement of decades-old statutes that prohibit the ownership of medical practices by corporations not owned by licensed doctors.
Thirty-three states plus the District of Columbia have rules on their books against the so-called corporate practice of medicine. But over the years, critics say, companies have successfully sidestepped bans on owning medical practices by buying or establishing local staffing groups that are nominally owned by doctors and restricting the physicians’ authority so they have no direct control.
These laws and regulations, which started appearing nearly a century ago, were meant to fight the commercialization of medicine, maintain the independence and authority of physicians, and prioritize the doctor-patient relationship over the interests of investors and shareholders.
Those campaigning for stiffer enforcement of the laws say that physician-staffing firms owned by private equity investors are the most egregious offenders. Private equity-backed staffing companies manage a quarter of the nation’s emergency rooms, according to a Raleigh, North Carolina-based doctor who runs a job site for ER physicians. The two largest are Nashville, Tennessee-based Envision Healthcare, owned by investment giant KKR & Co., and Knoxville, Tennessee-based TeamHealth, owned by Blackstone.
Court filings in multiple states, including California, Missouri, Texas, and Tennessee, have called out Envision and TeamHealth for allegedly using doctor groups as straw men to sidestep corporate practice laws. But those filings have typically been in financial cases involving wrongful termination, breach of contract, and overbilling.
Now, physicians and consumer advocates around the country are anticipating a California lawsuit against Envision, scheduled to start in January 2024 in federal court. The plaintiff in the case, Milwaukee-based American Academy of Emergency Medicine Physician Group, alleges that Envision uses shell business structures to retain de facto ownership of ER staffing groups, and it is asking the court to declare them illegal.
“We’re not asking them to pay money, and we will not accept being paid to drop the case,” said David Millstein, lead attorney for the plaintiff. “We are simply asking the court to ban this practice model.”
‘Possibility to Reverberate Throughout the Country’
The physician group believes a victory would lead to a prohibition of the practice across California — and not just in ERs, but for other staff provided by Envision and TeamHealth, including in anesthesiology and hospital medicine. The California Medical Association supports the lawsuit, saying it “will shape the boundaries of California’s prohibition on the corporate practice of medicine.”
The plaintiff — along with many doctors, nurses, and consumer advocates, as well as some lawmakers — hopes that success in the case will spur regulators and prosecutors in other states to take corporate medicine prohibitions more seriously. “Any decision anywhere in the country that says the corporate ownership of a medical practice is illegal has the possibility to reverberate throughout the country, absolutely — and I hope that it would,” said Julie Mayfield, a state senator in North Carolina.
But the push to reinvigorate laws restricting the corporate practice of medicine has plenty of skeptics, who view it as an effort to return to a golden era in medicine that is long gone or may never have existed to begin with. The genie is out of the bottle, they say, noting that the profit motive has penetrated every corner of health care and that nearly 70% of physicians in the U.S. are now employed by corporations and hospitals.
The corporate practice of medicine doctrine has “a very interesting and not a very flattering history,” said Barak Richman, a law professor at Duke University. “The medical profession was trying to assert its professional dominance that accrued a lot of benefits to itself in ways that were not terribly beneficial to patients or to the market.”
The California case involves Placentia-Linda Hospital in Orange County, where the plaintiff physician group lost its ER management contract to Envision. The complaint alleges that Envision uses the same business model at numerous hospitals around the state.
“Envision exercises profound and pervasive direct and indirect control and/or influence over the medical practice, making decisions which bear directly and indirectly on the practice of medicine, rendering physicians as mere employees, and diminishing physician independence and freedom from commercial interests,” according to the complaint.
Envision said the company is compliant with state laws and that its operating structure is common in the health care industry. “Legal challenges to that structure have proved meritless,” Envision wrote in an email. It added that “care decisions have and always will be between clinicians and patients.”
TeamHealth, an indirect target in the case, said its “world-class operating team” provides management services that “allow clinicians to focus on the practice of medicine and patient care through a structure commonly utilized by hospitals, health systems, and other providers across the country.”
State Rules Vary Widely
State laws and regulations governing the corporate practice of medicine vary widely on multiple factors, including whether there are exceptions for nonprofit organizations, how much of doctors’ revenue outside management firms can keep, who can own the equipment, and how violations are punished. New York, Texas, and California are considered to have among the toughest restrictions, while Florida and 16 other states have none.
Kirk Ogrosky, a partner at the law firm Goodwin Procter, said this kind of management structure predates the arrival of private equity in the industry. “I would be surprised if a company that is interested in investing in this space screwed up the formation documents; it would shock me,” Ogrosky said.
Private equity-backed firms have been attracted to emergency rooms in recent years because ERs are profitable and because they have been able to charge inflated amounts for out-of-network care — at least until a federal law cracked down on surprise billing. Envision and TeamHealth prioritize profits, critics say, by maximizing revenue, cutting costs, and consolidating smaller practices into ever-larger groups — to the point of regional dominance.
Envision and TeamHealth are privately owned, which makes it difficult to find reliable data on their finances and the extent of their market penetration.
Dr. Leon Adelman, co-founder and CEO of Ivy Clinicians, a Raleigh-based startup job site for emergency physicians, has spent 18 months piecing together data and found that private equity-backed staffing firms run 25% of the nation’s emergency rooms. TeamHealth and Envision have the two largest shares, with 8.6% and 8.3%, respectively, Adelman said.
Other estimates put private equity’s penetration of ERs at closer to 40%.
Doctors Push for Investigations
So far, efforts by emergency physicians and others to challenge private equity staffing firms over their alleged violations have yielded frustrating results.
An advocacy group called Take Medicine Back, formed last year by a handful of ER physicians, sent a letter in July to North Carolina Attorney General Josh Stein, asking him to investigate violations of the ban on the corporate practice of medicine. And because Stein holds a senior position at the National Association of Attorneys General, the letter also asked him to take the lead in persuading his fellow AGs to “launch a multi-state investigation into the widespread lack of enforcement” of corporate practice of medicine laws.
The group’s leader, Dr. Mitchell Li, said he was initially disappointed by the response he received from Stein’s office, which promised to review his request, saying it raised complex legal issues about the corporate practice of medicine in the state. But Li is now more hopeful, since he has secured a January appointment with officials in Stein’s office.
Dr. Robert McNamara, a co-founder of Li’s group and chair of emergency medicine at Temple University’s Lewis Katz School of Medicine, drafted complaints to the Texas Medical Board, along with Houston physician Dr. David Hoyer, asking the board to intervene against two doctors accused of fronting for professional entities controlled by Envision and TeamHealth. In both cases, the board declined to intervene.
McNamara, who serves as the chief medical officer of the physicians’ group in the California Envision case, also filed a complaint with Pennsylvania Attorney General Josh Shapiro, alleging that a group called Emergency Care Services of Pennsylvania PC, which was trying to contract with ER physicians of the Crozer Keystone Health System, was wholly owned by TeamHealth and serving as a shell to avoid scrutiny.
A senior official in Shapiro’s office responded, saying the complaint had been referred to two state agencies, but McNamara said he has heard nothing back in more than three years.
Differing Views on Private Equity’s Role
Proponents of private equity ownership say it has brought a lot of good to health care. Jamal Hagler, vice president of research at the American Investment Council, said private equity brings expertise to hospital systems, “whether it’s to hire new staff, grow and open up to new markets, integrate new technologies, or develop new technologies.”
But many physicians who have worked for private equity companies say their mission is not compatible with the best practice of medicine. They cite an emphasis on speed and high patient volume over safety; a preference for lesser-trained, cheaper medical providers; and treatment protocols unsuitable for certain patients.
Dr. Sean Jones, an emergency physician in Asheville, North Carolina, said his first full-time job was at a Florida hospital, where EmCare, a subsidiary of Envision, ran the emergency room. Jones said EmCare, in collaboration with the hospital’s owner, pushed doctors to meet performance goals related to wait times and treatments, which were not always good for patients.
For example, if a patient came in with abnormally high heart and respiratory rates — signs of sepsis — doctors were expected to give them large amounts of fluids and antibiotics within an hour, Jones said. But those symptoms could also be caused by a panic attack or heart failure.
“You don’t want to give a patient with heart failure 2 or 3 liters of fluid, and I would get emails saying, ‘You didn’t do this,’” he said. “Well, no, I didn’t, because the reason they couldn’t breathe was they had too much fluid in their lungs.”
Envision said the company’s 25,000 clinicians, “like all clinicians, exercise their independent judgment to provide quality, compassionate, clinically appropriate care.”
Jones felt otherwise. “We don’t need some MBAs telling us what to do,” he said.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/AWIP0Kc
 December 22, 2022
December 22, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
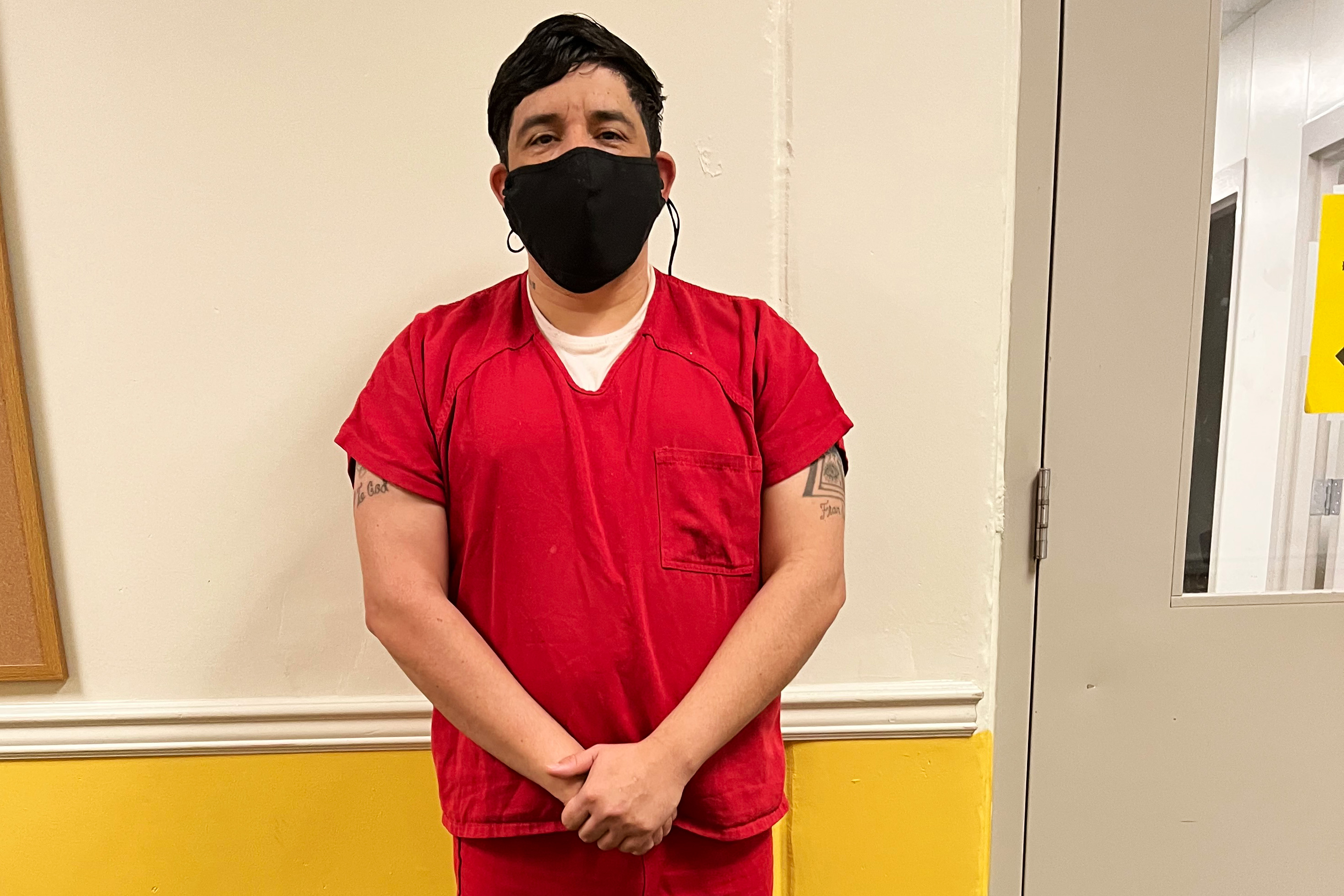
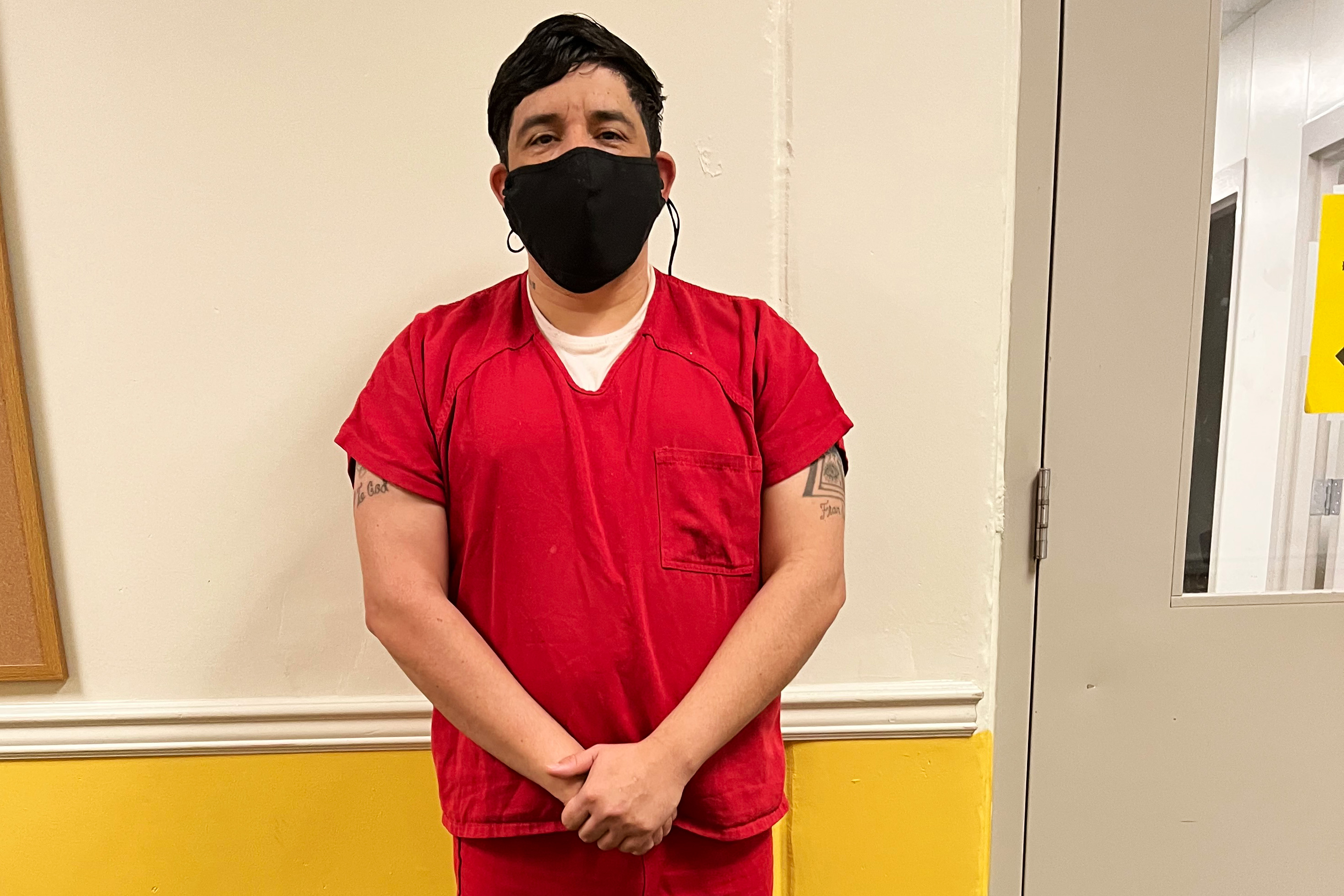
LUMPKIN, Ga. — In October, Yibran Ramirez-Cecena didn’t alert the staff at Stewart Detention Center to his cough and runny nose. Ramirez-Cecena, who had been detained at the immigration detention facility in southwestern Georgia since May, hid his symptoms, afraid he would be put in solitary confinement if he tested positive for covid-19.
“Honestly, I didn’t want to go spend 10 days by myself in a room — they call it the hole,” Ramirez-Cecena said. He is being held at the center as he waits to learn whether he will be deported to Mexico or can remain in the United States, where he has lived for more than two decades.
Shortly before Ramirez-Cecena got sick, officials from U.S. Immigration and Customs Enforcement at the facility denied his request for a medical release. He is HIV-positive, which is on the Centers for Disease Control and Prevention’s list of conditions that make a person more likely to get seriously ill from covid.
Now, heading into the third pandemic winter, he’s praying he doesn’t get covid while detained. “It is still scary,” he said.
Across the country, the chance of developing severe illness or dying from covid has fallen, a result of updated booster shots, at-home tests, and therapeutics. Most people can weigh the risks of attending gatherings or traveling. But for the roughly 30,000 people living in close quarters in the country’s network of immigration facilities, covid remains an ever-present threat.
ICE updated its pandemic guidance in November. But facilities have flouted past recommendations to use masks and protective equipment, to make testing and vaccines available, and to avoid the use of solitary confinement for quarantining, according to detainees, advocacy groups, and internal federal government reports.
Under ICE’s pandemic protocols, covid isolation, used to keep other detainees from falling ill, must be separate from disciplinary segregation. The agency didn’t address claims that facilities have used solitary confinement areas to isolate detainees who have tested positive for covid but said in a statement to KHN that detainees are placed in a “single, medical housing room” or a “medical airborne infection isolation room” when available.
Medical care in immigration detention facilities was deficient even before the pandemic. Then, in September, medically vulnerable people in ICE detention facilities lost a source of protection, with the expiration of a court order that had required federal immigration officials to consider releasing detainees with covid risks.
The agency has “completely given up on protecting people in detention from covid,” said Zoe Bowman, supervising attorney at Las Americas Immigrant Advocacy Center in El Paso, Texas.
The country’s use of immigration detention exploded in the late 1990s and rose even more after the creation of ICE in 2003. Detention facilities — made up of about 200 privately run complexes, ICE-run facilities, local jails, and prisons scattered across the country — hold adults who are not U.S. citizens while they contest or await deportation. The average length of stay in the 2022 federal fiscal year was about 22 days, according to the agency. Advocates for immigrants have long argued that people shouldn’t be detained and instead should be allowed to live in communities.
Stewart Detention Center, a vast complex surrounded by rows of barbed wire in Lumpkin’s forests, has one of the largest populations of detainees in the country. Four people in the center’s custody have died from covid since the start of the pandemic — the highest number of recorded covid deaths among detention centers.
When immigration officials transferred Cipriano Alvarez-Chavez to the Stewart center in August 2020, he was still relying on the mask he had after being released from federal prison in July, according to his daughter, Martha Chavez.
Ten days later, the 63-year-old lymphoma survivor was taken to a hospital in Columbus, 40 miles away, where he tested positive for covid, according to his death report. He died after spending more than a month on a ventilator.
“It was pure neglect,” his daughter said. His death “shattered our world.”
Two years after Alvarez-Chavez’s death, advocacy groups and detainees said ICE has not done enough to protect detainees from covid, a situation consistent with the facilities’ history of poor medical care and lack of hygiene. “It’s disheartening to see that no matter how bad things get, they don’t change,” said Dr. Amy Zeidan, an assistant professor at Emory University School of Medicine, who reviews detainee health records and performs medical evaluations for people seeking asylum.
A bipartisan Senate investigation revealed in November that women at Georgia’s Irwin County Detention Center “appear to have been subjected to excessive, invasive, and often unnecessary gynecological procedures.” At the Folkston Processing Center, also in Georgia, ICE did not respond to medical requests in a timely manner, had inadequate mental health care, and failed to meet basic hygiene standards, including working toilets, according to a June report from the Department of Homeland Security’s Office of Inspector General. And a July complaint filed by a group of advocacy organizations alleged that a nurse at the Stewart center sexually assaulted four women.
ICE defended its medical care in an emailed statement, saying that it spends more than $315 million on health care annually and ensures the provision of necessary and comprehensive medical services.
Still, many facilities are understaffed and ill-equipped to handle the long-term medical needs of the large detainee population, Zeidan said. Delayed care is common, specialty care is almost nonexistent, and access to therapeutics is limited, she said. Covid care is no different.
In its covid protocols, ICE recommends the use of monoclonal antibodies, which help the immune system respond more effectively to covid, for treatment. But it recognizes none of the other CDC-recommended treatments, including antivirals such as Paxlovid, which can reduce hospitalizations and deaths among covid patients.
“For decades, ICE has proven itself incapable and unwilling to ensure the health and safety of people in its custody,” said Sofia Casini, director of monitoring and community advocacy at Freedom for Immigrants, an advocacy group. “Covid-19 has only worsened this horrifying reality.”
Eleven people have died from covid in ICE custody. But that number may be an underestimate; advocates for detainees have accused the agency of releasing people or deporting them when they are seriously ill as a way to suppress the death statistics.
Before the pandemic, Johana Medina Leon was released from ICE custody four days before her death, according to a May article in the Los Angeles Times. She saw a doctor about six weeks after her first request, the article said, but ICE expedited her release only hours after her condition grew dire.
This fall, detainees being held at facilities across the country called Freedom for Immigrants’ detention hotline to complain about covid conditions, which vary facility to facility, Casini said. “Even in the same facility, it can change week to week,” she said.
Many people who had tested positive for covid were being held in the same cells as people who had tested negative, including people who were medically vulnerable, according to Casini. The group surveyed 89 people through its hotline this summer and found that about 30% of respondents had trouble accessing vaccines in detention.
Ramirez-Cecena said he was told that he’s eligible for a second covid booster shot but had yet to receive it as of December. A detainee at Moshannon Valley Processing Center in Pennsylvania said a guard was allowed to interact with detainees while visibly sick, said Brittney Bringuez, asylum program coordinator at Physicians for Human Rights, who visited the facility this fall.
The court order that required ICE to consider releasing people with covid risks has helped detainees with serious medical conditions, advocates said. Under the order, ICE released about 60,000 medically vulnerable detainees in two years, said Susan Meyers, senior staff attorney at the Southern Poverty Law Center, one of the advocacy groups that helped bring the lawsuit that resulted in the court order.
ICE said in a statement it will still consider covid risk factors as a reason for release. But lawyers said ICE facilities often failed to comply with the court order when it was in place.

Last year, ICE denied Ricardo Chambers’ request for release from Stewart Detention Center. Chambers, who is 40, has serious psychiatric illnesses, considered a risk factor under the court order. He also has trouble breathing and chokes in his sleep — the result of a nasal injury he sustained in an attack before he was detained. It has yet to be repaired during the two years he has been at the detention facility.
He has filed complaints about Stewart’s covid protocols, including crowded conditions and failures by staffers to wear masks or other protective equipment. In its denial of his release, ICE said Chambers was a threat to public safety because of his criminal history, according to his lawyer Erin Argueta, lead attorney for the Southern Poverty Law Center’s Southeast Immigrant Freedom Initiative office in Lumpkin. Chambers has served prison time for his criminal convictions, she said, and there’s a family in New York that would take him in.
Earlier this year, he was sent to solitary confinement for about 10 days after testing positive for covid, he said. But Chambers, who is fighting a deportation order to Jamaica, said his covid experience was no different from the other times he had been in solitary.
“You’ll be treated like an animal, caged, and for no fault of your own,” Chambers said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/va9uQPn
 December 22, 2022
December 22, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
LONDON — In the final days of 2020, the U.S. health insurer Centene made a swift incursion into Britain’s prized National Health Service, one of the world’s largest employers.
A Centene subsidiary, Operose Health, took over nearly three dozen medical practices in London — gateways for NHS care — in a deal worth tens of millions of dollars. The subsidiary became the largest private supplier of general practice services in the United Kingdom, with 67 practices accounting for 570,000 patients.
A local health commission, records show, signed off after a nine-minute review in a virtual hearing held the week before Christmas. Centene was not mentioned. Not a question was asked. It was the time of year — amid pandemic restraints — when official business in London gave way to fizzy cocktails and quiet glad tidings.
Within weeks, the acquisition set off alarms for Louise Irvine, an NHS doctor, who called it “privatization of the NHS by stealth.” Irvine, other practitioners, and residents supported a crowdfunded legal challenge to the takeover of AT Medics Holdings, the U.K. primary care company under contract to the NHS.
Centene is the largest privately managed care provider in the U.S. that offers government-sponsored insurance, such as Medicaid and Affordable Care Act plans, as well as health care to seniors, prisoners, military members, and veterans. Britons who protested its expansion saw a for-profit outsider with ambitions that could weaken the NHS. They worried Centene would decide on staffing to suit its bottom line. NHS contracts with doctors at set rates, and assistants are paid less; critics questioned whether the Centene deal would reduce more highly trained staff.
Then there was this: The corporation faced legal problems and had paid fines, since 2013, over noncompliance with state or federal Medicaid contracts or rules. By mid-2021, as its legal battle intensified in London, Centene was grappling with allegations of overbilling Medicaid for pharmacy services. It has since paid about $657 million to settle the accusations of 15 states. It faces investor lawsuits as well as overbilling allegations from several more states. Centene, based in Missouri, has denied wrongdoing.
Centene’s “suitability” for doing business with the NHS was not discussed in the virtual hearing. And because of technical limitations, members of the public could review the decision only through an audio recording, released online a day later.
“It was covid time,” Irvine, now retired, said with some frustration about the public meeting. “We believe NHS should be a public service, and it is being gradually eroded.”
Centene did not respond to requests to discuss its U.K. strategy. By July 2021, Centene’s interests also acquired Circle Health Group, a private health care group based in London with 50 hospitals.
Earlier this year, a judge ruled that the 2020 public meeting was conducted lawfully. The judge questioned the relevance of raising Centene’s liabilities; she noted the American company’s counsel had documented that its “financial position was strong” and that the insurer “continues to operate successfully in the U.S. health care market.”
Advocates for market-based efficiencies, including former NHS chiefs who were hired by Centene-related businesses, portray the managed-care titan as a change agent that can innovate and trim costs.
In October, an NHS care commission declined to renew a Centene contract for Hanley Primary Care Center in north London, which was part of the 2020 deal. The clinic was left with too few doctors, the Islington Tribune reported, and patient appointments had dropped by 270 a week, representing a “huge hole” in care since the acquisition. The NHS’ decision followed a BBC report in June about Operose staffing, in which clinic employees said the practice was short eight doctors and that less qualified workers, called physician associates, filled the gaps.
Operose spokesperson Stephen Webb, in an email, said the Hanley practice “is currently rated as ‘Good’ by the national regulator” and the contract would be reviewed next year. On its website, Operose calls the BBC report “sensational.” It adds that “we have a strong track record of performance, recruitment and investment in our staff and services.”
The Hanley decision is a small validation for Irvine and others who warned that efficiencies would degrade the quality of care.
“The whole ethos of the American system, well, it is fundamentally different than how we view care in the U.K.,” Irvine said. “Our values are free and accessible health care for all.”
Cultivating Ties in Government
Centene was eyeing the British health system in winter 2011, when it hosted health advisers from across Europe to tour its facilities in Spain’s seaside region of Valencia.
In March 2011, and again in 2015, representatives from Centene’s subsidiary Ribera Salud promoted its “pioneering approach” to caregiving at hospitals and treatment centers through a public-private partnership, according to an NHS advisory report.
Like Britain, Spain faces an aging population. The subsidiary promised a model for “efficient and effective healthcare” for patients who are government-supported or pay out-of-pocket. The government paid the provider a flat rate per patient each year, and Ribera Salud operated the sites and managed staff.
The approach intrigued British politicians and advisers, conservatives as well as liberals, eager to manage health care costs by encouraging competition.
Centene cultivated its image and relationships, launching the subsidiary Centene UK in 2016. Within months, it was hiring NHS administrators for its executive ranks. Among the highest-profile recruits: Samantha Jones, a nurse and the NHS England director of “new care models,” who had championed Centene’s work in Spain.
By 2019, Jones was named CEO of Centene UK. In 2021, she left to work for Prime Minister Boris Johnson as “an expert adviser for NHS transformation and social care.”
As Johnson’s premiership came under pressure, Jones was named chief of operations at No. 10 Downing St. She left when he resigned in July.
By then, Centene had a substantial U.K. foothold and other former NHS administrators had joined its top ranks. Contacted through LinkedIn, Jones said she was “not available to do any interviews.”
For consumers intent on preserving Britain’s national health care — or just understanding who owns what and where — Centene is difficult to track. It’s the same in the U.S., where the company has more than 300 subsidiaries. Names there typically lean into local iconography such as Peach State Health Plan of Georgia and Buckeye Community Health Plan of Ohio — with no mention of Centene.
In England, Jenny Shepherd, 72, has written about Centene and its subsidiaries for years. She set up a hyperlocal news site in 2012 to track public services amid government budget restraints. She soon focused on NHS. When Centene’s operations in Spain were being floated as a model for reform, Shepherd saw little coverage of it. “Journalism was lacking,” she said.
Shepherd scours regulatory filings for her posts, published under “NHS Matters.” Over years, she has documented a flowchart of sorts of Centene’s businesses. She said the company routinely recasts its corporate profile. From 2016 to 2018 alone, subsidiary names, addresses, and company directors changed often, she noted.
In 2018, Centene UK was listed as controlled by a Centene subsidiary, MH Services International Holdings. In November 2019, according to regulatory filings, Centene UK formally changed its name to Operose Health.
The practices acquired in 2020, however, were still identified in March 2021 as part of AT Medics Holdings. That filing, in U.K. government records, lists Operose Health as a board member.
Centene’s stake in Circle Health was laid out in December 2021 regulatory filings. Circle Health’s parent company in the U.K. is MH Services International (UK) Ltd., “with the ultimate parent being Centene Corporation,” records show.
Centene aims to wring profit from government-guaranteed payments, Shepherd said: “The English NHS is as big as the Chinese army, and it was clear that the Americans wanted to get their hands on it.”
Such guarantees have diminished, however, as health care costs have increased. The pandemic has propelled a two-year backlog for some treatments. For the first time in history, NHS nurses in England, Wales, and Northern Ireland went on strike in December, largely over pay. Ambulance drivers and paramedics in England and Wales followed suit. Military personnel were readied to take over some services.
‘Closer to the American Model’
The rise of for-profit providers within the British NHS has sparked incendiary debates, with brute questions about costs and motives. How much is spent on patients? How much is spent on services? And could market forces plow the national health landscape into a tiered system of care?
“We are seeing a shift in care access and waiting times, and a big rise in the number of people moving toward a private system,” said Chris Thomas, principal health fellow at the Institute for Public Policy Research think tank in London. “Britain already has the largest number of private patients in the G-7, and that brings us closer to the American model.”
Centene has been welcomed by some as a way “to ease burdens within a chronically overworked NHS,” Thomas said. “But it doesn’t seem optimal to have a corporation — a for-profit organization — coming in.”
Centene has seen limits to government guarantees, particularly in Spain.
Even as British health advisers visited Ribera Salud in 2011, the Spanish press was documenting financial missteps in the venture. Fees per patient, meant to cover access to universal care, had to be renegotiated. Directors and administrators moved between public-sector jobs and Ribera through what appeared to be an unchecked revolving door.
Anne Stafford, a finance professor at University of Manchester, examined the numbers behind the Ribera model. The rhetoric of savings never matched reality, she said, with no clear comparison offered of labor costs, financing, wage demand, and patient ratios between Spain and Britain.
Debates over how best to deliver care often lack rigor and consistency, she added. “People say they love their NHS, but they have no concept of how it is funded or how it operates,” she said. “That allows people with an agenda to get into the market.”
British politicians have seen health care as ripe for privatization since the late 1990s, she said, but “there is very little proper accountability” for whether “the private sector, in fact, is delivering value for money.”
NHS advisers also have questioned whether the two systems could be effectively compared: Invented after World War II, the NHS was so celebrated that in 2012 doctors and nurses marched in the opening ceremony of the London Olympics. Spain’s national health care emerged in the 1980s, after the death of dictator Gen. Francisco Franco, and it struggled with costs within its first decade. The Centene model in Valencia, reliant on bank financing, was implemented in 1999.
The report found differences in size and staffing of facilities as well as how care systems were integrated. Measuring possible cost savings was difficult and, the report said, “there are risks that these benefits may be hard to replicate.”
By December 2021, it was clear that Centene no longer regarded its Ribera operations as a moneymaker. It announced it would divest “non-core assets” to improve its profit margin.
Centene executives pointed investors to two international assets: Circle Health and Ribera.
Within months, the Spanish subsidiary was sold for an undisclosed figure, bundled with other health and diagnostic groups, to Vivalto Santé, the third-largest private hospital company in France. The acquisition was completed in November.
Centene, in a statement, described its excising of Ribera, with 10 hospitals, 1,650 beds, and 71 primary care and outpatient clinics, as a “significant milestone in our value creation plan.”
For now, it’s steaming ahead with its Circle Health venture. Its 1,900 beds delivered two-thirds of more than $2 billion in annual revenue, according to investor guidance in December 2021. It’s now the largest private hospital care provider in England.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/HCu3G2U
 December 22, 2022
December 22, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/AhOoLxC
 December 21, 2022
December 21, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

There’s no question that COVID-19 cut people off from one another. But for those who have long COVID, that disconnect has never really ended.
from WebMD Health https://ift.tt/2qrQaP9
 December 21, 2022
December 21, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/IcwpbJn
 December 21, 2022
December 21, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
Earlier this year, Grace Elizabeth Elliott got a mysterious hospital bill for medical care she had never received.
She soon discovered how far a clerical error can reach — even across a continent — and how frustrating it can be to fix.
During a college break in 2013, Elliott, then 22, began to feel faint and feverish while visiting her parents in Venice, Florida, about an hour south of Tampa. Her mother, a nurse, drove her to a facility that locals knew simply as Venice Hospital.
In the emergency department, Elliott was diagnosed with a kidney infection and held overnight before being discharged with a prescription for antibiotics, a common treatment for the illness.
“My hospital bill was about $100, which I remember because that was a lot of money for me as an undergrad,” said Elliott, now 31.
She recovered and eventually moved to California to teach preschool. Venice Regional Medical Center was bought by Community Health Systems, based in Franklin, Tennessee, in 2014 and eventually renamed ShorePoint Health Venice.
The kidney infection and overnight stay in the ER would have been little more than a memory for Elliott.
Then another bill came.
The Patients: Grace E. Elliott, 31, a preschool teacher living with her husband in San Francisco, and Grace A. Elliott, 81, a retiree in Venice, Florida.
Medical Services: For Grace E., an emergency department visit and overnight stay, plus antibiotics to treat a kidney infection in 2013. For Grace A., a shoulder replacement and rehabilitation services in 2021.
Service Provider: Venice Regional Medical Center, later renamed ShorePoint Health Venice.
Total Bill: $1,170, the patient’s responsibility for shoulder replacement services, after adjustments and payments of $13,210.21 by a health plan with no connection to Elliott. The initial charges were $123,854.14.
What Gives: This is a case of mistaken identity, a billing mystery that started at a hospital registration desk and didn’t end until months after the file had been handed over to a collection agency.
Early this year, Grace E. Elliott’s mother opened a bill from ShorePoint Health Venice that was addressed to her daughter and sought more than $1,000 for recent hospital services, Elliott said. She “immediately knew something was wrong.”
Months of sleuthing eventually revealed that the bill was meant for Grace Ann Elliott, a much older woman who underwent a shoulder replacement procedure and rehabilitation services at the Venice hospital last year.
Experts said that accessing the wrong patient’s file because of a name mix-up is a common error — but one for which safeguards, like checking a patient’s photo identification, usually exist.
The hospital had treated at least two Grace Elliotts. When Grace A. Elliott showed up for her shoulder replacement, a hospital employee pulled up Grace E. Elliott’s account by mistake.
“This is the kind of thing that can definitely happen,” said Shannon Hartsfield, a Florida attorney who specializes in health care privacy violations. (Hartsfield does not represent anyone involved in this case.) “All kinds of human errors happen. A worker can pull up the names, click the wrong button, and then not check [the current patient’s] date of birth to confirm.”
It was a seemingly obvious error: The younger Elliott was billed for a procedure she didn’t have by a hospital she had not visited in years. But it took her nearly a year of hours-long phone calls to undo the damage.

At first, worried that she had been the victim of identity theft, Grace E. Elliott contacted ShorePoint Health Venice and was bounced from one department to another. At one point, a billing employee disclosed to Elliott the birthdate the hospital had on file for the patient who had the shoulder replacement — it was not hers. Elliott then sent the hospital a copy of her ID.
It took weeks for an administrator at ShorePoint’s corporate office in Florida to admit the hospital’s error and promise to correct it.
In August, though, Grace E. Elliott received a notice that the corporate office had sold the debt to a collection agency called Medical Data Systems. Even though the hospital had acknowledged its error, the agency was coming after Grace E. Elliott for the balance due for Grace A. Elliott’s shoulder surgery.
“I thought, ‘Well, I’ll just work with them directly,’” Grace E. Elliott said.
Her appeal was denied. Medical Data Systems said in its denial letter that it had contacted the hospital and confirmed the name and address on file. The agency also included a copy of Grace A. Elliott’s expired driver license to Grace E. — along with several pages of the older woman’s medical information — in support of its conclusion.
“A collection agency, as a business associate of a hospital, has an obligation to ensure that the wrong patient’s information is not shared,” Hartsfield said.
In an email to KHN, Cheryl Spanier, a vice president of the collection agency, wrote that “MDS follows all state and federal rules and regulations.” Spanier declined to comment on Elliott’s case, saying she needed the written consent of both the health system and the patient to do so.
Elliott’s second appeal was also denied. She was told to contact the hospital to clear up the issue. But because the health system had long since sold the debt, Elliott said, she got no traction in trying to get ShorePoint Health Venice to help her. The hospital closed in September.
Resolution: In mid-November, shortly after a reporter contacted ShorePoint Health, which operates other hospitals and facilities in Florida, Grace E. Elliott received a call from Stanley Padfield, the Venice hospital’s outgoing privacy officer and director of health information management. “He said, ‘It’s taken care of,’” Elliott said, adding that she was relieved but skeptical. “I’ve heard that over and over.”
Elliott said Padfield told her that she had become listed as Grace A. Elliott’s guarantor, meaning she was legally responsible for the debt of a woman she had never met.
Elliott soon received a letter from Padfield stating that ShorePoint Health had removed her information from Grace A. Elliott’s account and confirmed that she had not been reported to any credit agencies. The letter said her information had been removed from the collection agency’s database and acknowledged that the hospital’s fix initially “was not appropriately communicated” to collections.
Padfield said the error started with a “registration clerk,” who he said had “received additional privacy education as a result of this incident.”
Devyn Brazelton, marketing coordinator for ShorePoint Health, told KHN the hospital believes the error was “an isolated incident.”
Using the date of birth provided by a hospital worker, Elliott was able to contact Grace A. Elliott and explain the mix-up.
“I’m a little upset right now,” Grace A. Elliott told KHN on the day she learned about the billing error and disclosure of her medical information.

The Takeaway: Grace E. Elliott said that when she asked Padfield, the Venice hospital’s outgoing privacy officer, whether she could have done something to fight such an obvious case of mistaken identity, he replied, “Probably not.”
This, experts said, is the dark secret of identity issues: Once a mistake has been entered into a database, it can be remarkably difficult to fix. And such incorrect information can live for generations.
For patients, that means it’s crucial to review the information on patient portals — the online medical profiles many providers use to manage things like scheduling appointments, organizing medical records, and answering patient questions.
One downside of electronic medical records is that errors spread easily and repeat frequently. It is important to challenge and correct errors in medical records early and forcefully, with every bit of documentation available. That is true whether the problem is an incorrect name, a medication no longer (or never) taken, or an inaccurate diagnosis.
The process of amending a record can be “very involved,” Hartsfield said. “But with patients able now to see more and more of their medical records, they are going to want those amendments, and health systems and their related entities need to get prepared for that.”
Grace A. Elliott told KHN that she had received a call from ShorePoint Health in the previous few months indicating that she owed money for her shoulder replacement.
She asked for a copy of the bill, she told KHN. Months after she asked, it still hadn’t arrived.
Bill of the Month is a crowdsourced investigation by KHN and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/gEzWRoH
 December 20, 2022
December 20, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

U.S. health officials report that deaths of teens from drug overdoses soared starting in late 2019, and though they appear to be on the decline, they remain much higher than in 2019.
from WebMD Health https://ift.tt/hIsoEOZ
 December 20, 2022
December 20, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments
Habits are what can turn your goal or resolution into reality. Find out how to make good ones and break bad habits – for keeps.
from WebMD Health https://ift.tt/JLbdNQl
 December 20, 2022
December 20, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments

When you have diabetes, regular eye exams are crucial to look for diabetic retinopathy, the leading cause of blindness in adults in the United States. One of the country's leading eye specialists explains why.
from WebMD Health https://ift.tt/tVBs2xl
 December 20, 2022
December 20, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
When a group of physicians gathered in Washington state for an annual meeting, one made a startling revelation: If you ever want to know when, how — and where — to kill someone, I can tell you, and you’ll get away with it. No problem.
That’s because the expertise and availability of coroners, who determine cause of death in criminal and unexplained cases, vary widely across Washington, as they do in many other parts of the country.
“A coroner doesn’t have to ever have taken a science class in their life,” said Nancy Belcher, chief executive officer of the King County Medical Society, the group that met that day.
Her colleague’s startling comment launched her on a four-year journey to improve the state’s archaic death investigation system, she said. “These are the people that go in, look at a homicide scene or death, and say whether there needs to be an autopsy. They’re the ultimate decision-maker,” Belcher added.
Each state has its own laws governing the investigation of violent and unexplained deaths, and most delegate the task to cities, counties, and regional districts. The job can be held by an elected coroner as young as 18 or a highly trained physician appointed as medical examiner. Some death investigators work for elected sheriffs who try to avoid controversy or owe political favors. Others own funeral homes and direct bodies to their private businesses.
Overall, it’s a disjointed and chronically underfunded system — with more than 2,000 offices across the country that determine the cause of death in about 600,000 cases a year.
“There are some really egregious conflicts of interest that can arise with coroners,” said Justin Feldman, a visiting professor at Harvard University’s FXB Center for Health and Human Rights.
Belcher’s crusade succeeded in changing some aspects of Washington’s coroner system when state lawmakers approved a new law last year, but efforts to reform death investigations in California, Georgia, and Illinois have recently failed.
Rulings on causes of death are often not cut-and-dried and can be controversial, especially in police-involved deaths such as the 2020 killing of George Floyd. In that case, Minnesota’s Hennepin County medical examiner ruled Floyd’s death a homicide but indicated a heart condition and the presence of fentanyl in his system may have been factors. Pathologists hired by Floyd’s family said he died from lack of oxygen when a police officer kneeled on his neck and back.
In a recent California case, the Sacramento County coroner’s office ruled that Lori McClintock, the wife of congressman Tom McClintock, died from dehydration and gastroenteritis in December 2021 after ingesting white mulberry leaf, a plant not considered toxic to humans. The ruling triggered questions by scientists, doctors, and pathologists about the decision to link the plant to her cause of death. When asked to explain how he made the connection, Dr. Jason Tovar, the chief forensic pathologist who reports to the coroner, said he reviewed literature about the plant online using WebMD and Verywell Health.
The various titles used by death investigators don’t distinguish the discrepancies in their credentials. Some communities rely on coroners, who may be elected or appointed to their offices, and may — or may not — have medical training. Medical examiners, on the other hand, are typically doctors who have completed residencies in forensic pathology.
In 2009, the National Research Council recommended that states replace coroners with medical examiners, describing a system “in need of significant improvement.”
Massachusetts was the first state to replace coroners with medical examiners statewide in 1877. As of 2019, 22 states and the District of Columbia had only medical examiners, 14 states had only coroners, and 14 had a mix, according to the Centers for Disease Control and Prevention.
The movement to convert the rest of the country’s death investigators from coroners to medical examiners is waning, a casualty of coroners’ political might in their communities and the additional costs needed to pay for medical examiners’ expertise.
The push is now to better train coroners and give them greater independence from other government agencies.
“When you try to remove them, you run into a political wall,” said Dr. Jeffrey Jentzen, a former medical examiner for the city of Milwaukee and the author of “Death Investigation in America: Coroners, Medical Examiners, and the Pursuit of Medical Certainty.”
“You can’t kill them, so you have to help train them,” he added.
There wouldn’t be enough medical examiners to meet demand anyway, in part because of the time and expense it takes to become trained after medical school, said Dr. Kathryn Pinneri, president of the National Association of Medical Examiners. She estimates there are about 750 full-time pathologists nationwide and about 80 job openings. About 40 forensic pathologists are certified in an average year, she said.
“There’s a huge shortage,” Pinneri said. “People talk about abolishing the coroner system, but it’s really not feasible. I think we need to train coroners. That’s what will improve the system.”
Her association has called for coroners and medical examiners to function independently, without ties to other government or law enforcement agencies. A 2011 survey by the group found that 82% of the forensic pathologists who responded had faced pressure from politicians or the deceased person’s relatives to change the reported cause or manner of death in a case.
Dr. Bennet Omalu, a former chief forensic pathologist in California, resigned five years ago over what he described as interference by the San Joaquin County sheriff to protect law enforcement officers.
“California has the most backward system in death investigation, is the most backward in forensic science and in forensic medicine,” Omalu testified before the state Senate Governance and Finance Committee in 2018.
San Joaquin County has since separated its coroner duties from the sheriff’s office.
The Golden State is one of three states that allow sheriffs to also serve as coroners, and all but 10 of California’s 58 counties combine the offices. Legislative efforts to separate them have failed at least twice, most recently this year.
AB 1608, spearheaded by state Assembly member Mike Gipson (D-Carson), cleared that chamber but failed to get enough votes in the Senate.
“We thought we had a modest proposal. That it was a first step,” said Robert Collins, who advocated for the bill and whose 30-year-old stepson, Angelo Quinto, died after being restrained by Antioch police in December 2020.
The Contra Costa County coroner’s office, part of the sheriff’s department, blamed Quinto’s death on “excited delirium,” a controversial finding sometimes used to explain deaths in police custody. The finding has been rejected by the American Medical Association and the World Health Organization.
Lawmakers “didn’t want their names behind something that will get the sheriffs against them,” Collins said. “Just having that opposition is enough to scare a lot of politicians.”
The influential California State Sheriffs’ Association and the California State Coroners Association opposed the bill, describing the “massive costs” to set up stand-alone coroner offices.
Many Illinois counties also said they would shoulder a financial burden under similar legislation introduced last year by state Rep. Maurice West, a Democrat. His more sweeping bill would have replaced coroners with medical examiners.
Rural counties, in particular, complained about their tight budgets and killed his bill before it got a committee hearing, he said.
“When something like this affects rural areas, if they push back a little bit, we just stop,” West said.
Proponents of overhauling the system in Washington state — where in small, rural counties, the local prosecutor doubles as the coroner — faced similar hurdles.
The King County Medical Society, which wrote the legislation to divorce the two, said the system created a conflict of interest. But small counties worried they didn’t have the money to hire a coroner.
So, lawmakers struck a deal with the counties to allow them to pool their resources and hire shared contract coroners in exchange for ending the dual role for prosecutors by 2025. The bill, HB 1326, signed last year by Democratic Gov. Jay Inslee, also requires more rigorous training for coroners and medical examiners.
“We had some hostile people that we talked to that really just felt that we were gunning for them, and we absolutely were not,” Belcher said. “We were just trying to figure out a system that I think anybody would agree needed to be overhauled.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/Lrul5wY
 December 19, 2022
December 19, 2022 Rose
Rose Healthy Living, WebMD Health
Healthy Living, WebMD Health No comments
No comments
What's being done to help people with psoriatic disease? We get a look at the ever-changing picture from a rheumatologist.
from WebMD Health https://ift.tt/m7GgfVl
 December 19, 2022
December 19, 2022 Rose
Rose Health - The New York Times, NYT > Health
Health - The New York Times, NYT > Health No comments
No comments
from NYT > Health https://ift.tt/27g6Hjd
 December 19, 2022
December 19, 2022 Rose
Rose Health News, Kaiser Health News
Health News, Kaiser Health News No comments
No comments
A Montana addiction clinic’s plan to give people with substance use disorders as much as $1,966.50 in gift cards and vouchers to follow its treatment program is raising questions about the use of financial incentives with patients.
The tug of war over the effective but largely unregulated tool is playing out in the northwestern Montana town of Kalispell, where a local government grant is financing rewards for people who stick with treatment provided by the outpatient clinic Oxytocin.
Such incentives have gained momentum among individual health clinics and states in recent years. Since 2021, California, Washington, and Wisconsin have started incentive-based programs. Some private clinics offer their own rewards, such as giving clients gift cards for successfully passing a drug test.
In Montana, where Republican Gov. Greg Gianforte has made expanding behavioral health care a priority, a state pilot program offers prizes to people with addictions who stay off drugs. Oxytocin’s program, while funded by a government grant, is separate from the pilot program.
The allowable value of prizes that go to beneficiaries of federal health programs, like Medicaid, is a legal gray area, so totals vary from one program to the next.
The federal government doesn’t have a rule limiting the size of financial awards or guidelines detailing best practices, said Richard Rawson, professor emeritus in the Department of Psychiatry and Biobehavioral Sciences at UCLA.
“People don’t know where to look to understand this method, so states and providers make it up as they go along,” said Rawson, who has studied such incentives for about 20 years.
In June, Montana’s Flathead County awarded the Kalispell clinic, Oxytocin, a $500,000 grant funded by state alcohol tax revenue. Of that money, $300,000 was earmarked for incentives for participants to attend treatment, according to the clinic’s proposal. It proposed that over a 20-week treatment course, participants could earn as much as $1,966.50 in either gift cards or vouchers.
In Oxytocin’s program, a client has multiple chances each week to earn an incentive by passing urine tests and attending treatment. The dollar amount increases with consecutive successes.
The county chose Oxytocin from among four clinics that applied for the substance use treatment funding. By November, at least one complaint had been filed with state agencies accusing Oxytocin of committing Medicaid fraud by paying its clients — most of whom are Medicaid recipients — that high of a reward to attend treatment.
Oxytocin clinical director Pamela Liccardi declined requests to be interviewed but said in an email that the business had done nothing wrong. “There is a reason the community stands behind us and it is not because we do fraudulent things,” she wrote.
Research shows that motivational incentives, called contingency management, can reduce the number of days someone takes illicit stimulants, such as methamphetamines, and can promote abstaining from other substances, such as opiates, by reinforcing healthy behavior with prizes, privileges, or cash.
“We know people are dying from methamphetamine now,” said Michael McDonell, a community and behavioral health professor at Washington State University, who has helped states create incentive programs. “Contingency management is the only evidence-based intervention for methamphetamine use disorder. It’s the only intervention that’s shown consistently to be impactful.”
But clinicians are wary of running afoul of a 1972 federal anti-kickback statute that prohibits offering something of value to a federal beneficiary, such as a Medicaid recipient, to induce them to select a particular provider.
There are “safe harbors” meant to protect certain programs that are unlikely to lead to corruption. But a February legal advisory opinion from the U.S. Department of Health and Human Services’ Office of Inspector General said those exceptions don’t include incentives aimed at beneficiaries. Federal officials have long been concerned that those types of offers could lead to fraud and abuse.
“Programs that involve giving remuneration to beneficiaries can corrupt medical care decision-making, which could result in overutilization, increased costs, steering to particular providers or suppliers, or inappropriate medical choices,” the advisory opinion says.
Whether programs that offer incentives to beneficiaries of federal health programs violate the anti-kickback law is decided on a case-by-case basis, the inspector general’s office wrote. Among the factors is the value of the incentives, says the advisory opinion, without setting a specific benchmark.
Rawson and other researchers said most providers consider a total of $75 per client a year to be safe, based on a 2016 statement from the inspector general’s office on inexpensive gifts to beneficiaries.
However, Rawson said research indicates that amount is likely too low to work well as an incentive. Another annual limit that programs encounter is $600 per client, the threshold for reporting taxable income to the IRS. Exceeding that amount could cause beneficiaries to exceed Medicaid income limits, which could lead to loss of coverage.
Last year, Montana officials began a pilot program that expands stimulant use disorder treatments and includes incentives.
Tammera Nauts, with the Montana Primary Care Association, said the state was careful to avoid raising any red flags for the federal government in the rules it set for the state program. For example, participating clinics can’t give patients prizes to participate in treatment the federal government covers, such as therapy sessions. State pilot sites’ incentives also can’t go over $315 total per beneficiary a year — a cap Montana was allowed through a Centers for Medicare & Medicaid Services waiver.
Providers may offer their own rewards program without going through the state, and Nauts said Oxytocin is not one of the pilot sites tethered to Montana’s program.
KHN obtained a copy of a complaint filed against Oxytocin. In addition to the allegations of Medicaid fraud, it accuses Oxytocin of having several providers who offer services outside of their area of expertise or without a license. The document KHN received did not include the name of the person who filed the complaint, and state officials declined to provide details.
The complaint was filed with the state’s Department of Public Health and Human Services and Department of Justice. Health department spokesperson Jon Ebelt said it would be premature to comment on the case before the review is complete. Department of Justice spokesperson Emilee Cantrell said the agency’s Medicaid fraud unit was working with the health department but said she couldn’t provide details because an active complaint is considered confidential criminal justice information.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
from Kaiser Health News https://ift.tt/rfAHwxs





 Rose
Rose